| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 5718592 | 1411254 | 2017 | 7 صفحه PDF | دانلود رایگان |
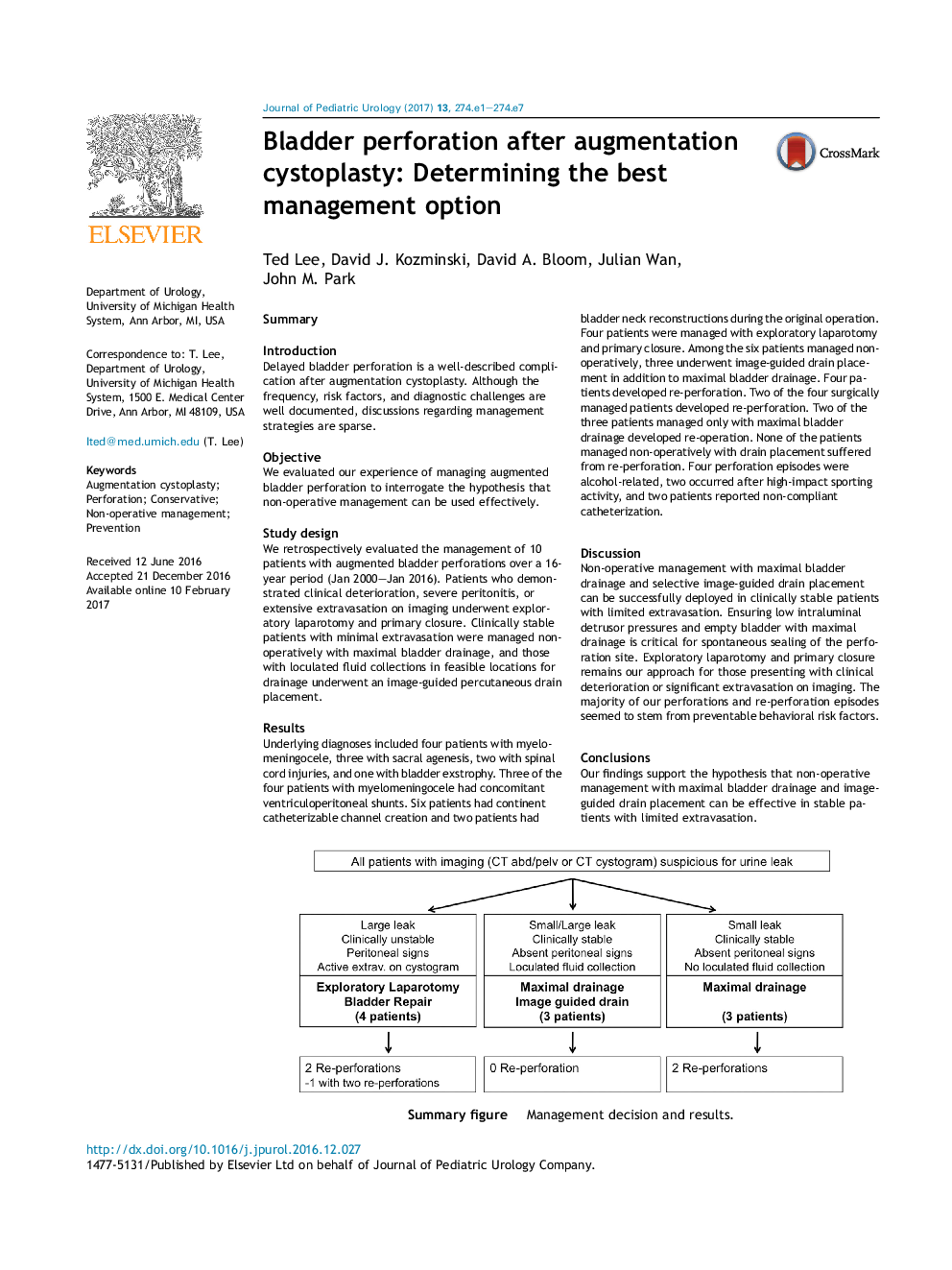
SummaryIntroductionDelayed bladder perforation is a well-described complication after augmentation cystoplasty. Although the frequency, risk factors, and diagnostic challenges are well documented, discussions regarding management strategies are sparse.ObjectiveWe evaluated our experience of managing augmented bladder perforation to interrogate the hypothesis that non-operative management can be used effectively.Study designWe retrospectively evaluated the management of 10 patients with augmented bladder perforations over a 16-year period (Jan 2000-Jan 2016). Patients who demonstrated clinical deterioration, severe peritonitis, or extensive extravasation on imaging underwent exploratory laparotomy and primary closure. Clinically stable patients with minimal extravasation were managed non-operatively with maximal bladder drainage, and those with loculated fluid collections in feasible locations for drainage underwent an image-guided percutaneous drain placement.ResultsUnderlying diagnoses included four patients with myelomeningocele, three with sacral agenesis, two with spinal cord injuries, and one with bladder exstrophy. Three of the four patients with myelomeningocele had concomitant ventriculoperitoneal shunts. Six patients had continent catheterizable channel creation and two patients had bladder neck reconstructions during the original operation. Four patients were managed with exploratory laparotomy and primary closure. Among the six patients managed non-operatively, three underwent image-guided drain placement in addition to maximal bladder drainage. Four patients developed re-perforation. Two of the four surgically managed patients developed re-perforation. Two of the three patients managed only with maximal bladder drainage developed re-operation. None of the patients managed non-operatively with drain placement suffered from re-perforation. Four perforation episodes were alcohol-related, two occurred after high-impact sporting activity, and two patients reported non-compliant catheterization.DiscussionNon-operative management with maximal bladder drainage and selective image-guided drain placement can be successfully deployed in clinically stable patients with limited extravasation. Ensuring low intraluminal detrusor pressures and empty bladder with maximal drainage is critical for spontaneous sealing of the perforation site. Exploratory laparotomy and primary closure remains our approach for those presenting with clinical deterioration or significant extravasation on imaging. The majority of our perforations and re-perforation episodes seemed to stem from preventable behavioral risk factors.ConclusionsOur findings support the hypothesis that non-operative management with maximal bladder drainage and image-guided drain placement can be effective in stable patients with limited extravasation.276Summary figure. Management decision and results.
Journal: Journal of Pediatric Urology - Volume 13, Issue 3, June 2017, Pages 274.e1-274.e7