| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 5718607 | 1411254 | 2017 | 7 صفحه PDF | دانلود رایگان |
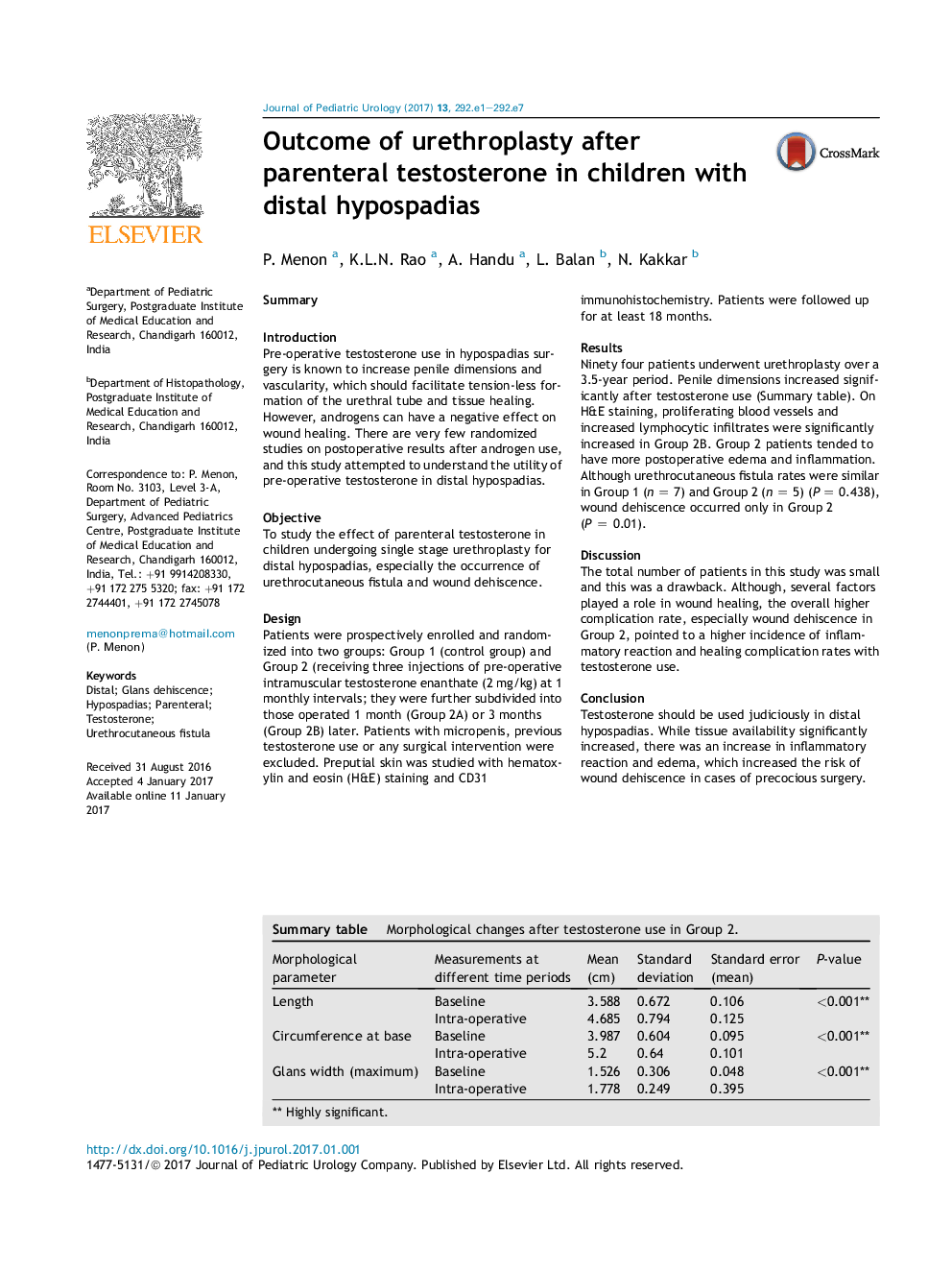
SummaryIntroductionPre-operative testosterone use in hypospadias surgery is known to increase penile dimensions and vascularity, which should facilitate tension-less formation of the urethral tube and tissue healing. However, androgens can have a negative effect on wound healing. There are very few randomized studies on postoperative results after androgen use, and this study attempted to understand the utility of pre-operative testosterone in distal hypospadias.ObjectiveTo study the effect of parenteral testosterone in children undergoing single stage urethroplasty for distal hypospadias, especially the occurrence of urethrocutaneous fistula and wound dehiscence.DesignPatients were prospectively enrolled and randomized into two groups: Group 1 (control group) and Group 2 (receiving three injections of pre-operative intramuscular testosterone enanthate (2 mg/kg) at 1 monthly intervals; they were further subdivided into those operated 1 month (Group 2A) or 3 months (Group 2B) later. Patients with micropenis, previous testosterone use or any surgical intervention were excluded. Preputial skin was studied with hematoxylin and eosin (H&E) staining and CD31 immunohistochemistry. Patients were followed up for at least 18 months.ResultsNinety four patients underwent urethroplasty over a 3.5-year period. Penile dimensions increased significantly after testosterone use (Summary table). On H&E staining, proliferating blood vessels and increased lymphocytic infiltrates were significantly increased in Group 2B. Group 2 patients tended to have more postoperative edema and inflammation. Although urethrocutaneous fistula rates were similar in Group 1 (n = 7) and Group 2 (n = 5) (P = 0.438), wound dehiscence occurred only in Group 2 (P = 0.01).DiscussionThe total number of patients in this study was small and this was a drawback. Although, several factors played a role in wound healing, the overall higher complication rate, especially wound dehiscence in Group 2, pointed to a higher incidence of inflammatory reaction and healing complication rates with testosterone use.ConclusionTestosterone should be used judiciously in distal hypospadias. While tissue availability significantly increased, there was an increase in inflammatory reaction and edema, which increased the risk of wound dehiscence in cases of precocious surgery.Summary table. Morphological changes after testosterone use in Group 2.Morphological parameterMeasurements at different time periodsMean (cm)Standard deviationStandard error (mean)P-valueLengthBaseline3.5880.6720.106<0.001**Intra-operative4.6850.7940.125Circumference at baseBaseline3.9870.6040.095<0.001**Intra-operative5.20.640.101Glans width (maximum)Baseline1.5260.3060.048<0.001**Intra-operative1.7780.2490.395** Highly significant.
Journal: Journal of Pediatric Urology - Volume 13, Issue 3, June 2017, Pages 292.e1-292.e7