| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2743309 | Anaesthesia & Intensive Care Medicine | 2007 | 4 Pages |
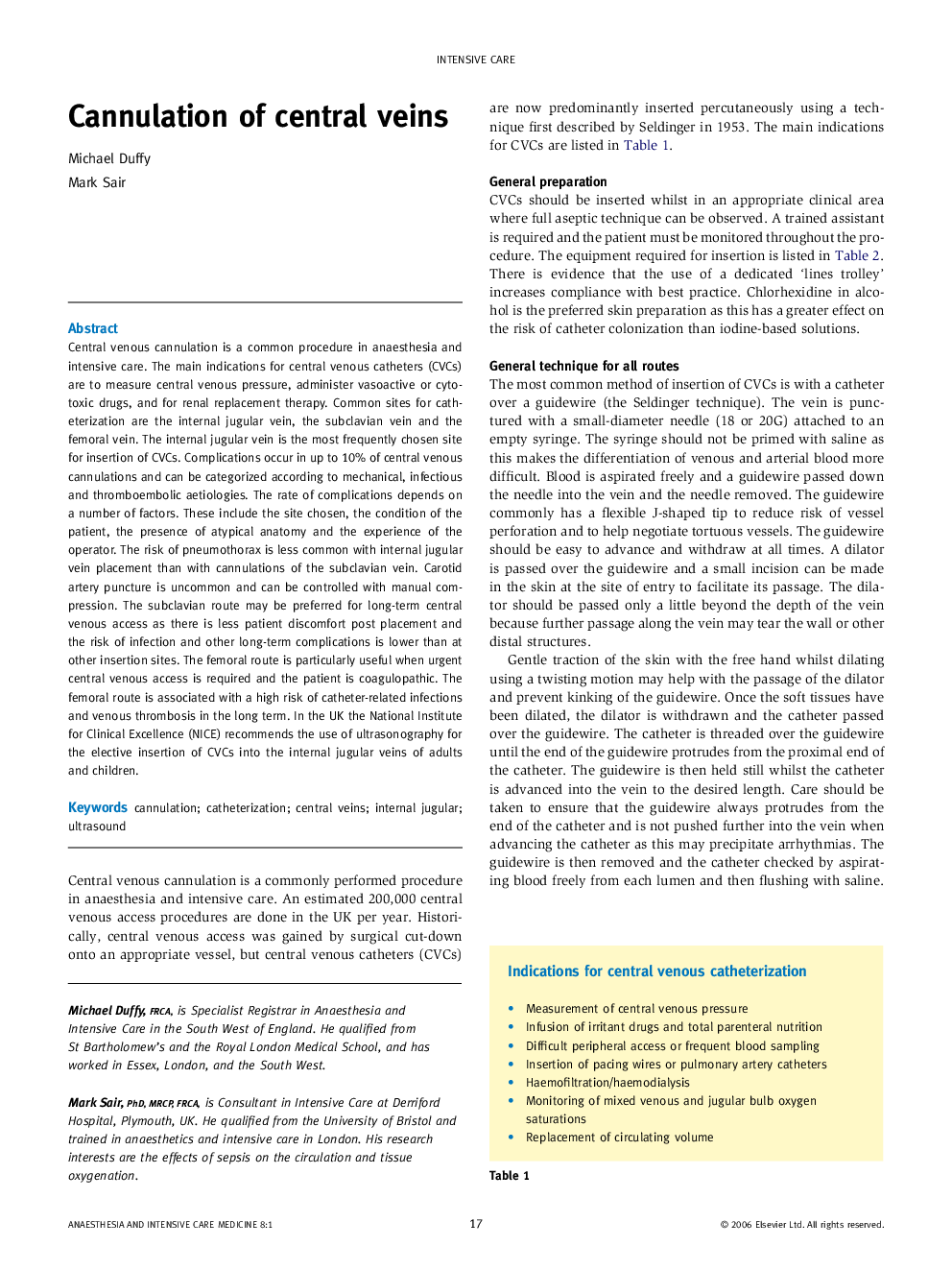
Central venous cannulation is a common procedure in anaesthesia and intensive care. The main indications for central venous catheters (CVCs) are to measure central venous pressure, administer vasoactive or cytotoxic drugs, and for renal replacement therapy. Common sites for catheterization are the internal jugular vein, the subclavian vein and the femoral vein. The internal jugular vein is the most frequently chosen site for insertion of CVCs. Complications occur in up to 10% of central venous cannulations and can be categorized according to mechanical, infectious and thromboembolic aetiologies. The rate of complications depends on a number of factors. These include the site chosen, the condition of the patient, the presence of atypical anatomy and the experience of the operator. The risk of pneumothorax is less common with internal jugular vein placement than with cannulations of the subclavian vein. Carotid artery puncture is uncommon and can be controlled with manual compression. The subclavian route may be preferred for long-term central venous access as there is less patient discomfort post placement and the risk of infection and other long-term complications is lower than at other insertion sites. The femoral route is particularly useful when urgent central venous access is required and the patient is coagulopathic. The femoral route is associated with a high risk of catheter-related infections and venous thrombosis in the long term. In the UK the National Institute for Clinical Excellence (NICE) recommends the use of ultrasonography for the elective insertion of CVCs into the internal jugular veins of adults and children.