| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2743324 | Anaesthesia & Intensive Care Medicine | 2009 | 5 Pages |
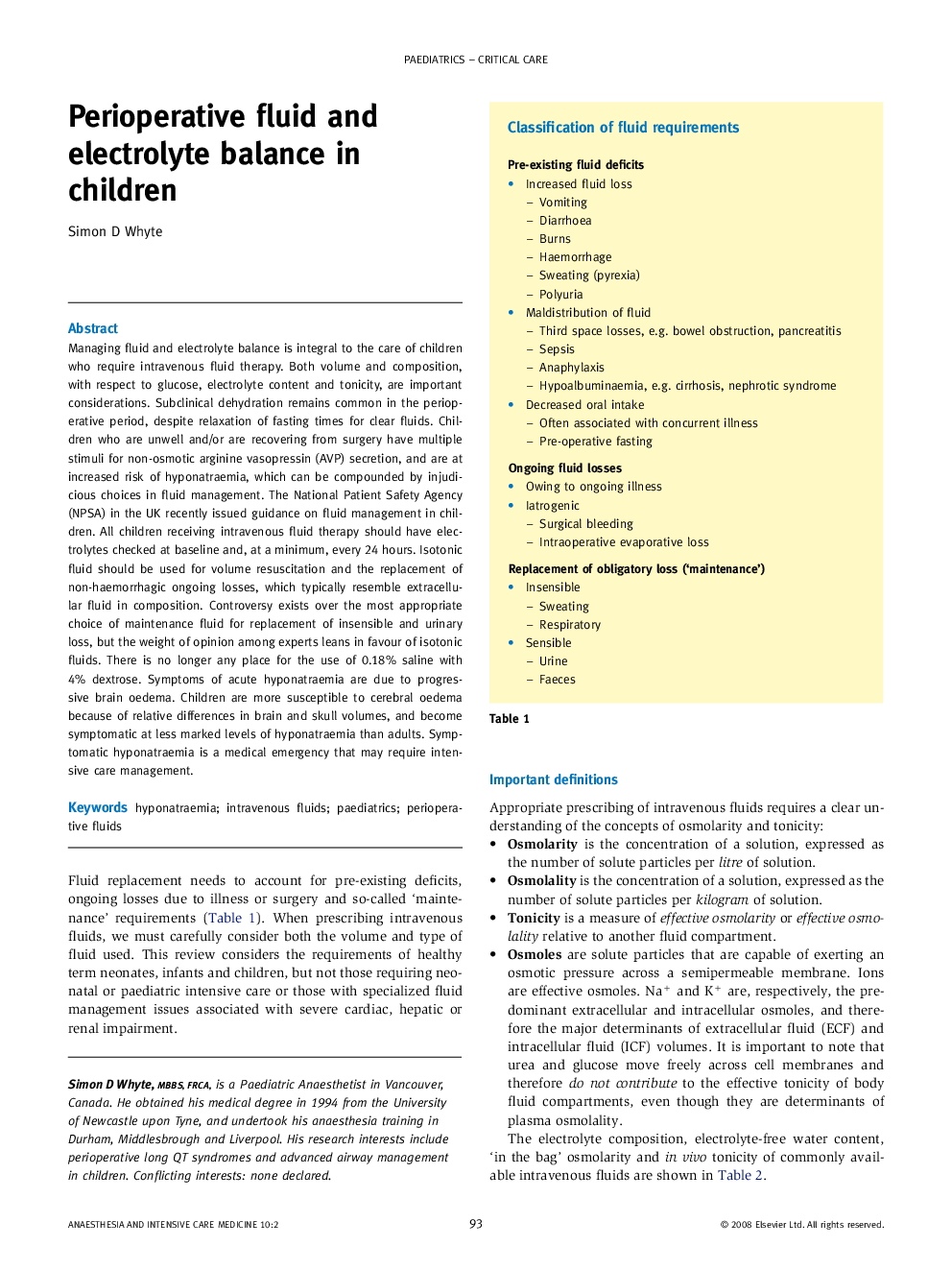
Managing fluid and electrolyte balance is integral to the care of children who require intravenous fluid therapy. Both volume and composition, with respect to glucose, electrolyte content and tonicity, are important considerations. Subclinical dehydration remains common in the perioperative period, despite relaxation of fasting times for clear fluids. Children who are unwell and/or are recovering from surgery have multiple stimuli for non-osmotic arginine vasopressin (AVP) secretion, and are at increased risk of hyponatraemia, which can be compounded by injudicious choices in fluid management. The National Patient Safety Agency (NPSA) in the UK recently issued guidance on fluid management in children. All children receiving intravenous fluid therapy should have electrolytes checked at baseline and, at a minimum, every 24 hours. Isotonic fluid should be used for volume resuscitation and the replacement of non-haemorrhagic ongoing losses, which typically resemble extracellular fluid in composition. Controversy exists over the most appropriate choice of maintenance fluid for replacement of insensible and urinary loss, but the weight of opinion among experts leans in favour of isotonic fluids. There is no longer any place for the use of 0.18% saline with 4% dextrose. Symptoms of acute hyponatraemia are due to progressive brain oedema. Children are more susceptible to cerebral oedema because of relative differences in brain and skull volumes, and become symptomatic at less marked levels of hyponatraemia than adults. Symptomatic hyponatraemia is a medical emergency that may require intensive care management.