| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2743546 | Anaesthesia & Intensive Care Medicine | 2009 | 4 Pages |
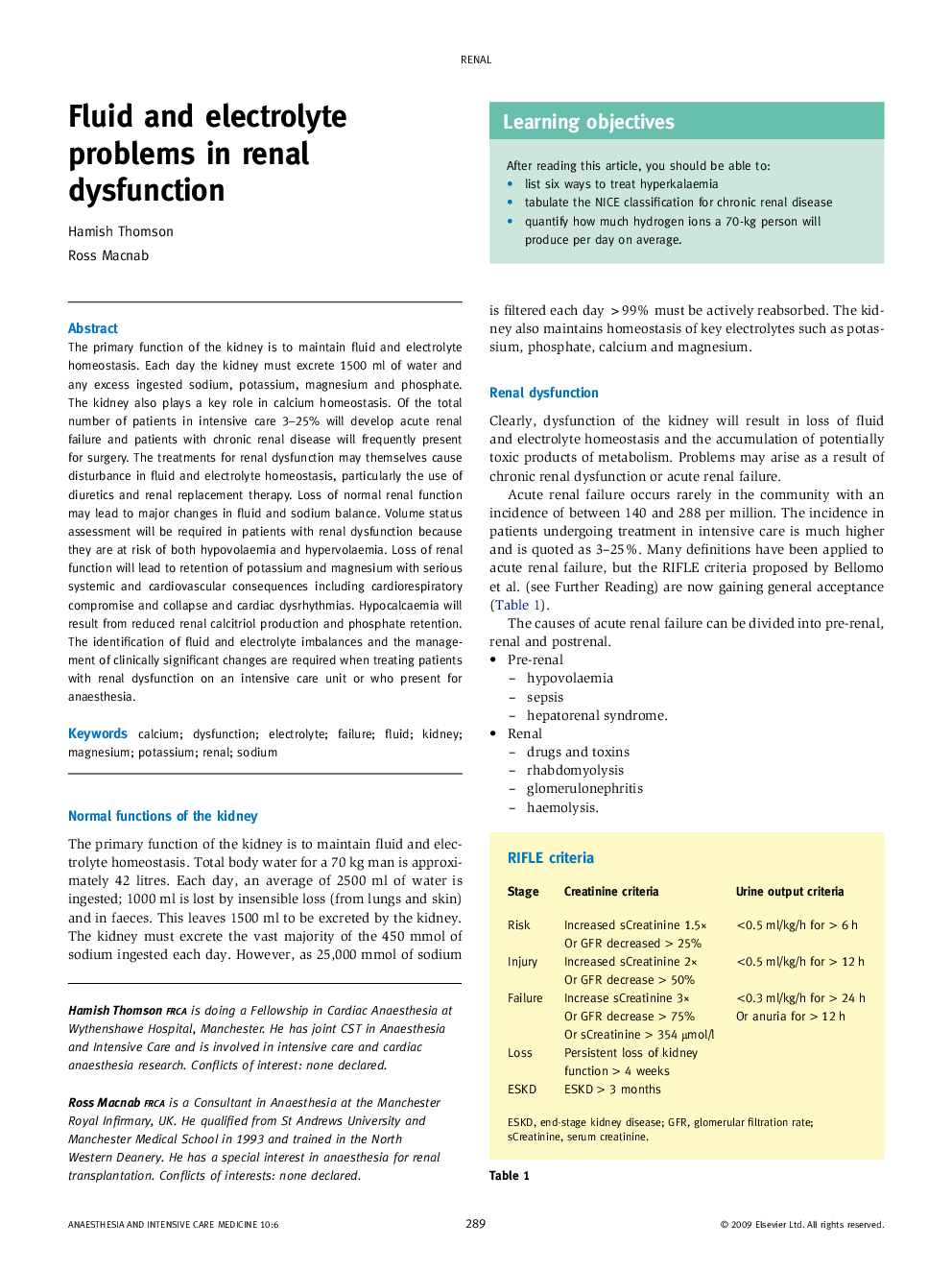
The primary function of the kidney is to maintain fluid and electrolyte homeostasis. Each day the kidney must excrete 1500 ml of water and any excess ingested sodium, potassium, magnesium and phosphate. The kidney also plays a key role in calcium homeostasis. Of the total number of patients in intensive care 3–25% will develop acute renal failure and patients with chronic renal disease will frequently present for surgery. The treatments for renal dysfunction may themselves cause disturbance in fluid and electrolyte homeostasis, particularly the use of diuretics and renal replacement therapy. Loss of normal renal function may lead to major changes in fluid and sodium balance. Volume status assessment will be required in patients with renal dysfunction because they are at risk of both hypovolaemia and hypervolaemia. Loss of renal function will lead to retention of potassium and magnesium with serious systemic and cardiovascular consequences including cardiorespiratory compromise and collapse and cardiac dysrhythmias. Hypocalcaemia will result from reduced renal calcitriol production and phosphate retention. The identification of fluid and electrolyte imbalances and the management of clinically significant changes are required when treating patients with renal dysfunction on an intensive care unit or who present for anaesthesia.