| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2743748 | Anaesthesia & Intensive Care Medicine | 2008 | 4 Pages |
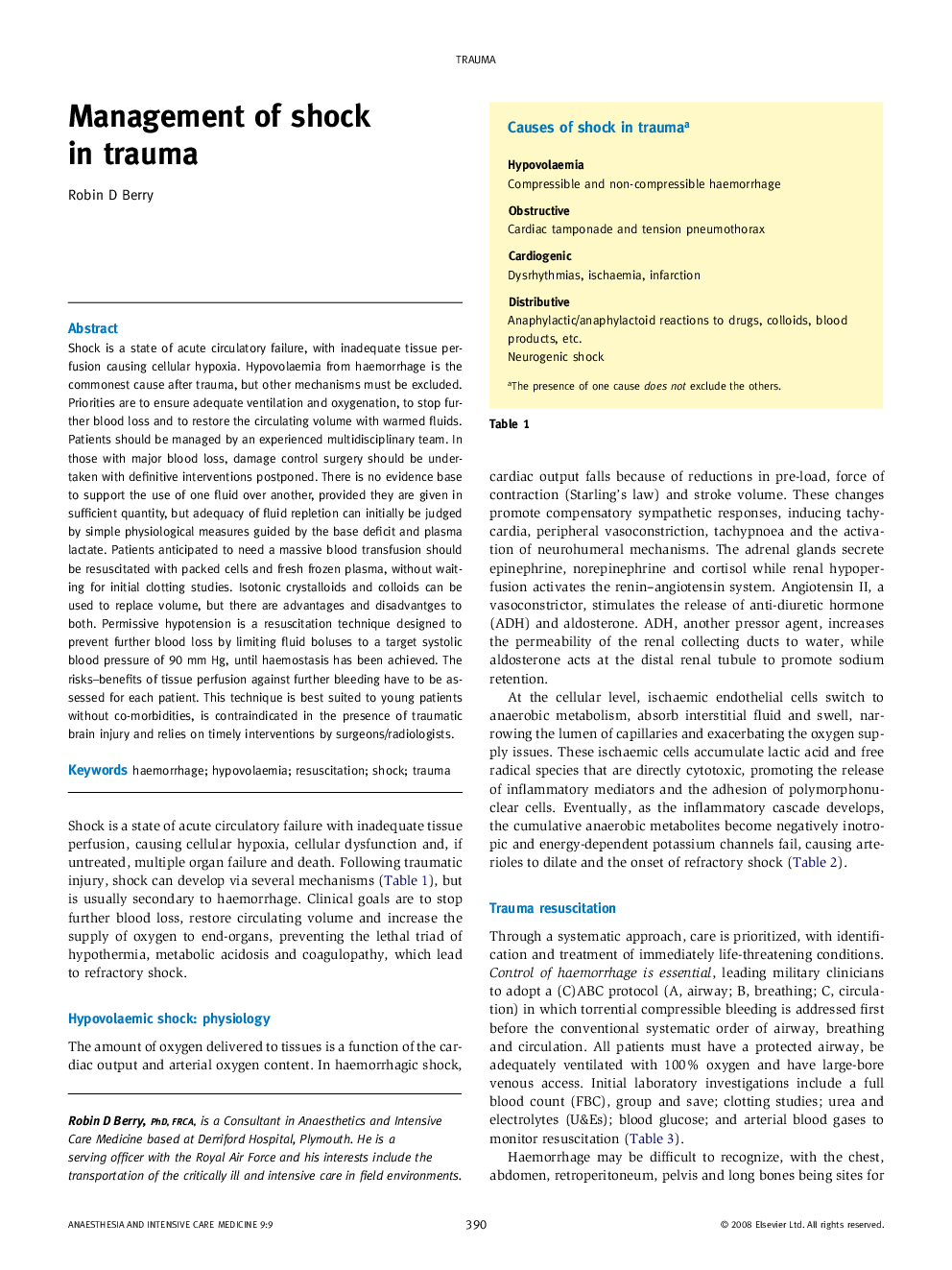
Shock is a state of acute circulatory failure, with inadequate tissue perfusion causing cellular hypoxia. Hypovolaemia from haemorrhage is the commonest cause after trauma, but other mechanisms must be excluded. Priorities are to ensure adequate ventilation and oxygenation, to stop further blood loss and to restore the circulating volume with warmed fluids. Patients should be managed by an experienced multidisciplinary team. In those with major blood loss, damage control surgery should be undertaken with definitive interventions postponed. There is no evidence base to support the use of one fluid over another, provided they are given in sufficient quantity, but adequacy of fluid repletion can initially be judged by simple physiological measures guided by the base deficit and plasma lactate. Patients anticipated to need a massive blood transfusion should be resuscitated with packed cells and fresh frozen plasma, without waiting for initial clotting studies. Isotonic crystalloids and colloids can be used to replace volume, but there are advantages and disadvantges to both. Permissive hypotension is a resuscitation technique designed to prevent further blood loss by limiting fluid boluses to a target systolic blood pressure of 90 mm Hg, until haemostasis has been achieved. The risks–benefits of tissue perfusion against further bleeding have to be assessed for each patient. This technique is best suited to young patients without co-morbidities, is contraindicated in the presence of traumatic brain injury and relies on timely interventions by surgeons/radiologists.