| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2792413 | Cell Metabolism | 2016 | 16 Pages |
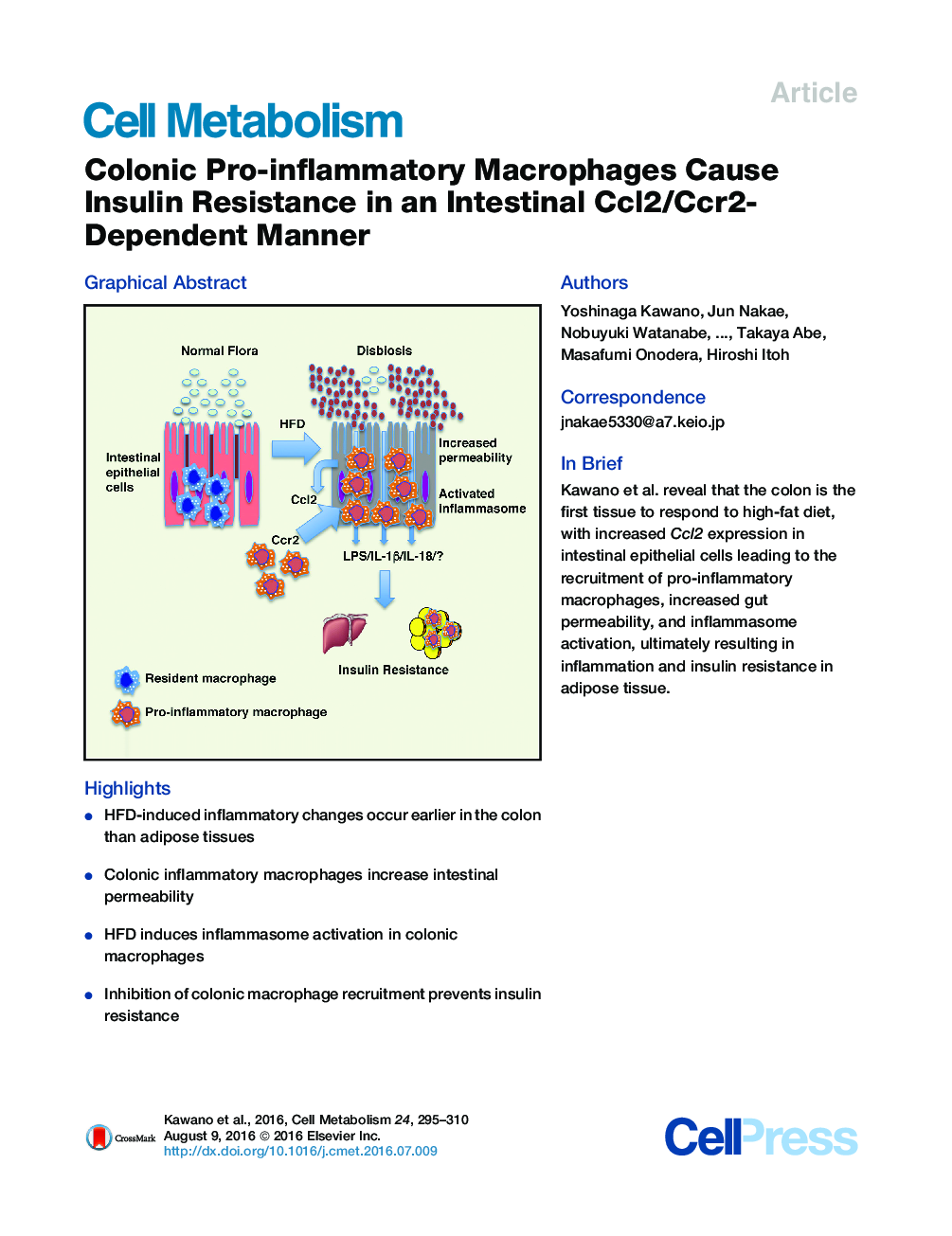
•HFD-induced inflammatory changes occur earlier in the colon than adipose tissues•Colonic inflammatory macrophages increase intestinal permeability•HFD induces inflammasome activation in colonic macrophages•Inhibition of colonic macrophage recruitment prevents insulin resistance
SummaryHigh-fat diet (HFD) induces low-grade chronic inflammation and insulin resistance. However, little is known about the mechanism underlying HFD-induced chronic inflammation in peripheral insulin-responsive tissues. Here, we show that colonic pro-inflammatory macrophages regulate insulin sensitivity under HFD conditions. To investigate the pathophysiological role of colonic macrophages, we generated macrophage-specific chemokine (C-C Motif) receptor 2 (Ccr2) knockout (M-Ccr2KO) and intestinal epithelial cell-specific tamoxifen-inducible Ccl2 knockout (Vil-Ccl2KO) mice. Both strains exhibited similar body weight to control under HFD. However, they exhibited decreased infiltration of colonic pro-inflammatory macrophages, decreased intestinal permeability, and inactivation of the colonic inflammasome. Interestingly, they showed significantly improved glucose tolerance and insulin sensitivity with decreased chronic inflammation of adipose tissue. Therefore, inhibition of pro-inflammatory macrophage infiltration prevents HFD-induced insulin resistance and could be a novel therapeutic approach for type 2 diabetes.
Graphical AbstractFigure optionsDownload full-size imageDownload high-quality image (232 K)Download as PowerPoint slide