| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2792553 | Cell Metabolism | 2015 | 12 Pages |
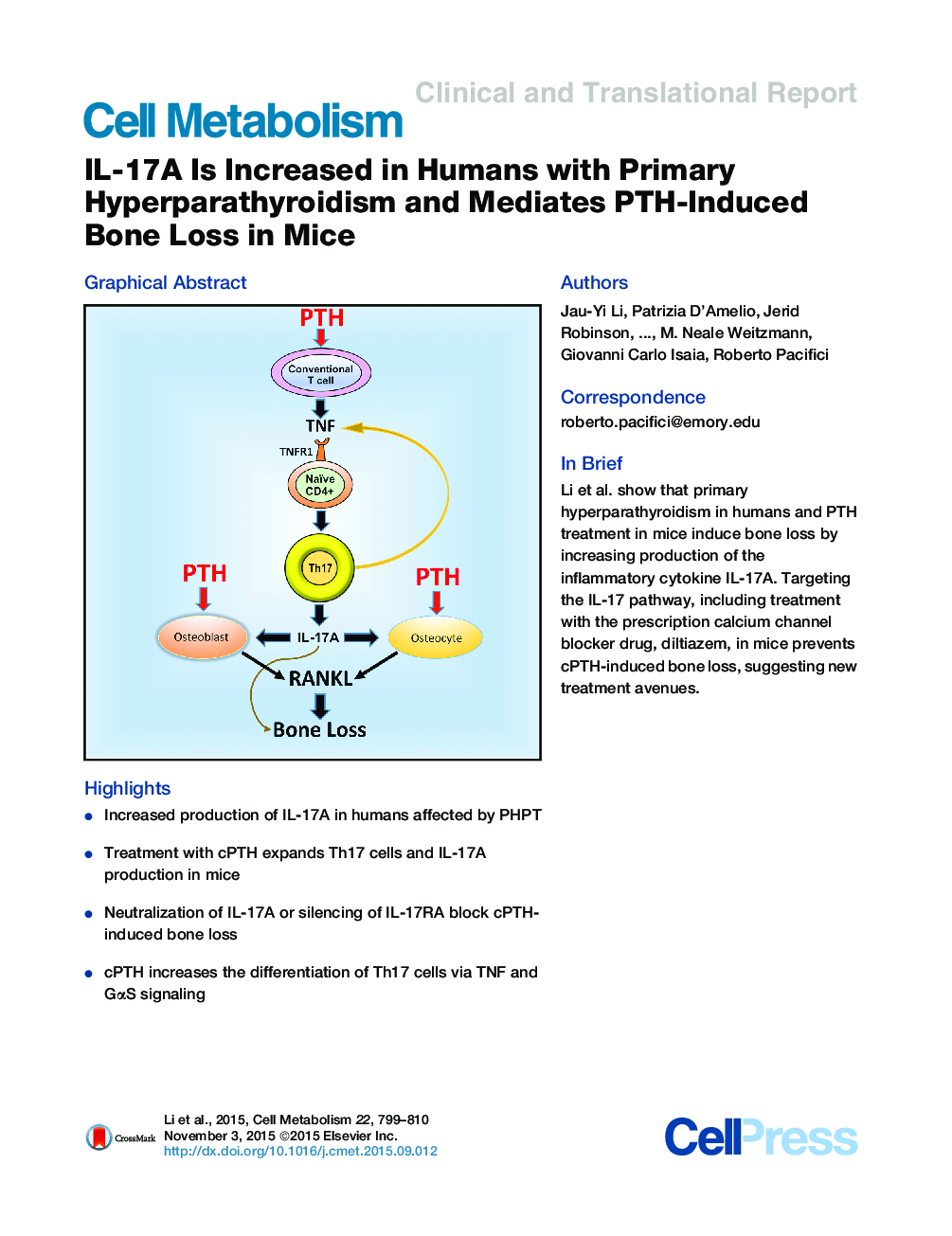
•Increased production of IL-17A in humans affected by PHPT•Treatment with cPTH expands Th17 cells and IL-17A production in mice•Neutralization of IL-17A or silencing of IL-17RA block cPTH-induced bone loss•cPTH increases the differentiation of Th17 cells via TNF and GαS signaling
SummaryPrimary hyperparathyroidism (PHPT) is a common cause of bone loss that is modeled by continuous PTH (cPTH) infusion. Here we show that the inflammatory cytokine IL-17A is upregulated by PHPT in humans and cPTH in mice. In humans, IL-17A is normalized by parathyroidectomy. In mice, treatment with anti-IL-17A antibody and silencing of IL-17A receptor IL-17RA prevent cPTH-induced osteocytic and osteoblastic RANKL production and bone loss. Mechanistically, cPTH stimulates conventional T cell production of TNFα (TNF), which increases the differentiation of IL-17A-producing Th17 cells via TNF receptor 1 (TNFR1) signaling in CD4+ cells. Moreover, cPTH enhances the sensitivity of naive CD4+ cells to TNF via GαS/cAMP/Ca2+ signaling. Accordingly, conditional deletion of GαS in CD4+ cells and treatment with the calcium channel blocker diltiazem prevents Th17 cell expansion and blocks cPTH-induced bone loss. Neutralization of IL-17A and calcium channel blockers may thus represent novel therapeutic strategies for hyperparathyroidism.
Graphical AbstractFigure optionsDownload full-size imageDownload high-quality image (161 K)Download as PowerPoint slide