| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 4292715 | Journal of the American College of Surgeons | 2013 | 7 Pages |
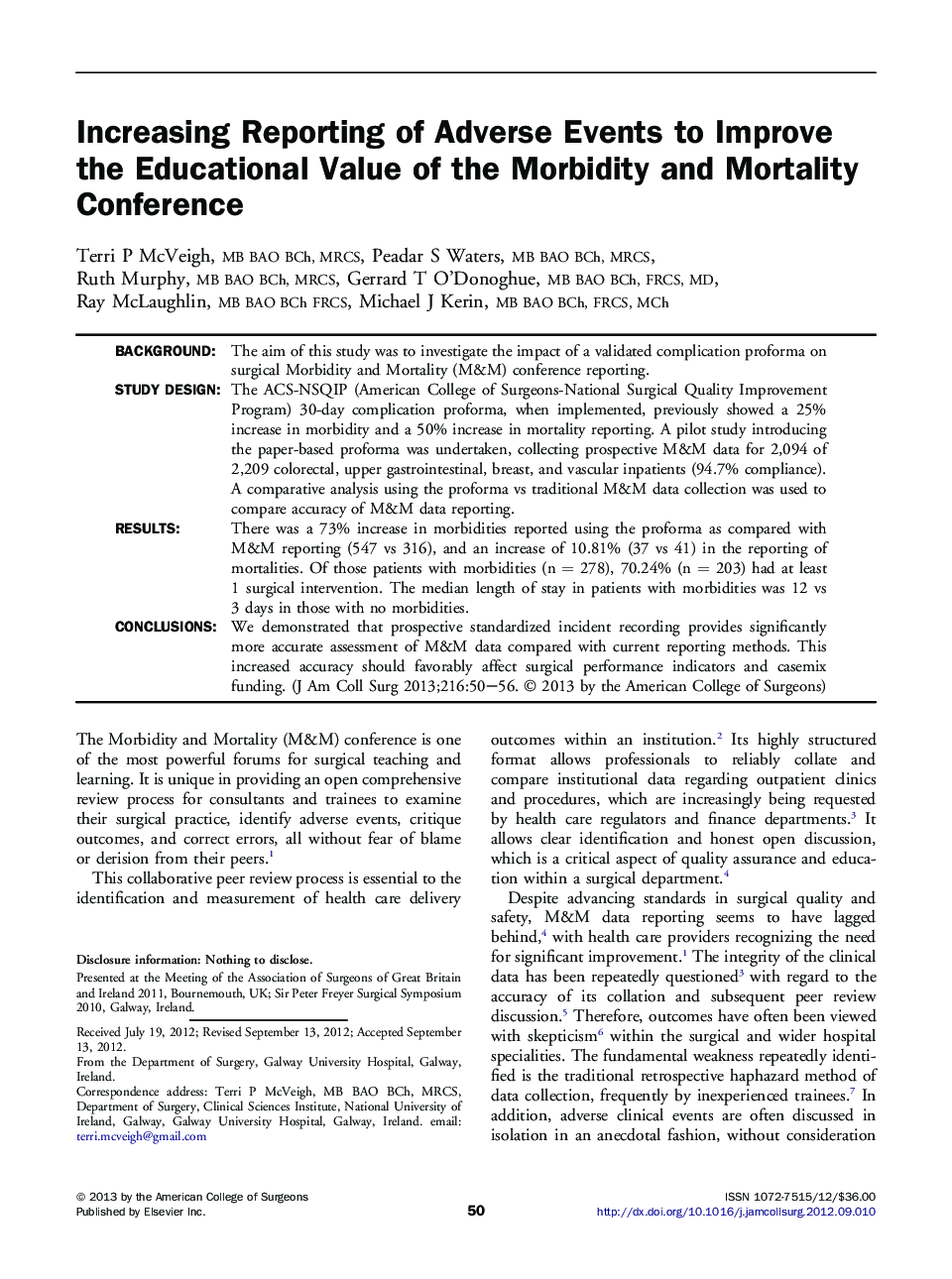
BackgroundThe aim of this study was to investigate the impact of a validated complication proforma on surgical Morbidity and Mortality (M&M) conference reporting.Study DesignThe ACS-NSQIP (American College of Surgeons-National Surgical Quality Improvement Program) 30-day complication proforma, when implemented, previously showed a 25% increase in morbidity and a 50% increase in mortality reporting. A pilot study introducing the paper-based proforma was undertaken, collecting prospective M&M data for 2,094 of 2,209 colorectal, upper gastrointestinal, breast, and vascular inpatients (94.7% compliance). A comparative analysis using the proforma vs traditional M&M data collection was used to compare accuracy of M&M data reporting.ResultsThere was a 73% increase in morbidities reported using the proforma as compared with M&M reporting (547 vs 316), and an increase of 10.81% (37 vs 41) in the reporting of mortalities. Of those patients with morbidities (n = 278), 70.24% (n = 203) had at least 1 surgical intervention. The median length of stay in patients with morbidities was 12 vs 3 days in those with no morbidities.ConclusionsWe demonstrated that prospective standardized incident recording provides significantly more accurate assessment of M&M data compared with current reporting methods. This increased accuracy should favorably affect surgical performance indicators and casemix funding.