| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 4293011 | Journal of the American College of Surgeons | 2011 | 8 Pages |
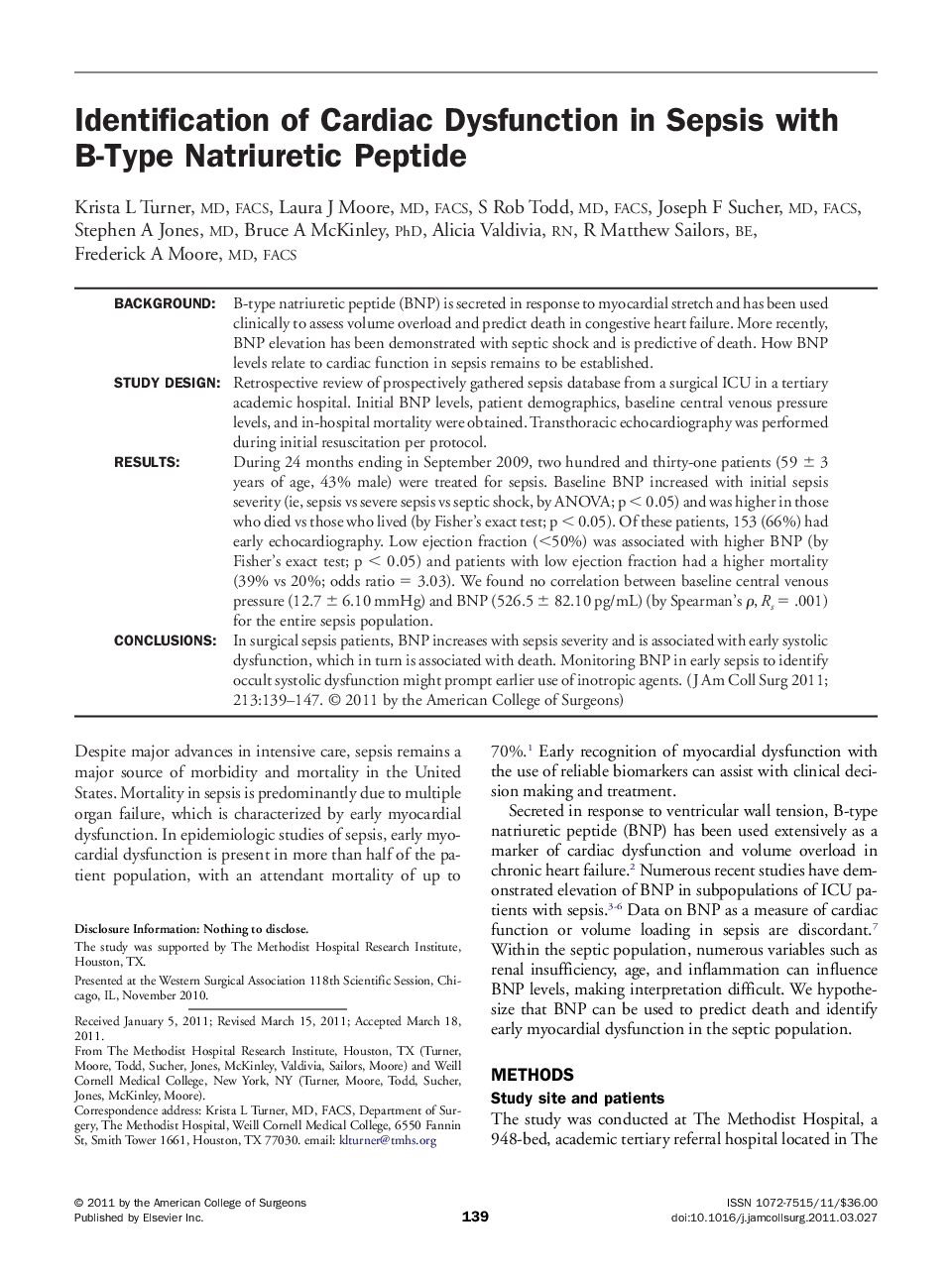
BackgroundB-type natriuretic peptide (BNP) is secreted in response to myocardial stretch and has been used clinically to assess volume overload and predict death in congestive heart failure. More recently, BNP elevation has been demonstrated with septic shock and is predictive of death. How BNP levels relate to cardiac function in sepsis remains to be established.Study DesignRetrospective review of prospectively gathered sepsis database from a surgical ICU in a tertiary academic hospital. Initial BNP levels, patient demographics, baseline central venous pressure levels, and in-hospital mortality were obtained. Transthoracic echocardiography was performed during initial resuscitation per protocol.ResultsDuring 24 months ending in September 2009, two hundred and thirty-one patients (59 ± 3 years of age, 43% male) were treated for sepsis. Baseline BNP increased with initial sepsis severity (ie, sepsis vs severe sepsis vs septic shock, by ANOVA; p < 0.05) and was higher in those who died vs those who lived (by Fisher's exact test; p < 0.05). Of these patients, 153 (66%) had early echocardiography. Low ejection fraction (<50%) was associated with higher BNP (by Fisher's exact test; p < 0.05) and patients with low ejection fraction had a higher mortality (39% vs 20%; odds ratio = 3.03). We found no correlation between baseline central venous pressure (12.7 ± 6.10 mmHg) and BNP (526.5 ± 82.10 pg/mL) (by Spearman's ρ, Rs = .001) for the entire sepsis population.ConclusionsIn surgical sepsis patients, BNP increases with sepsis severity and is associated with early systolic dysfunction, which in turn is associated with death. Monitoring BNP in early sepsis to identify occult systolic dysfunction might prompt earlier use of inotropic agents.