| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 5718730 | Journal of Pediatric Urology | 2016 | 6 Pages |
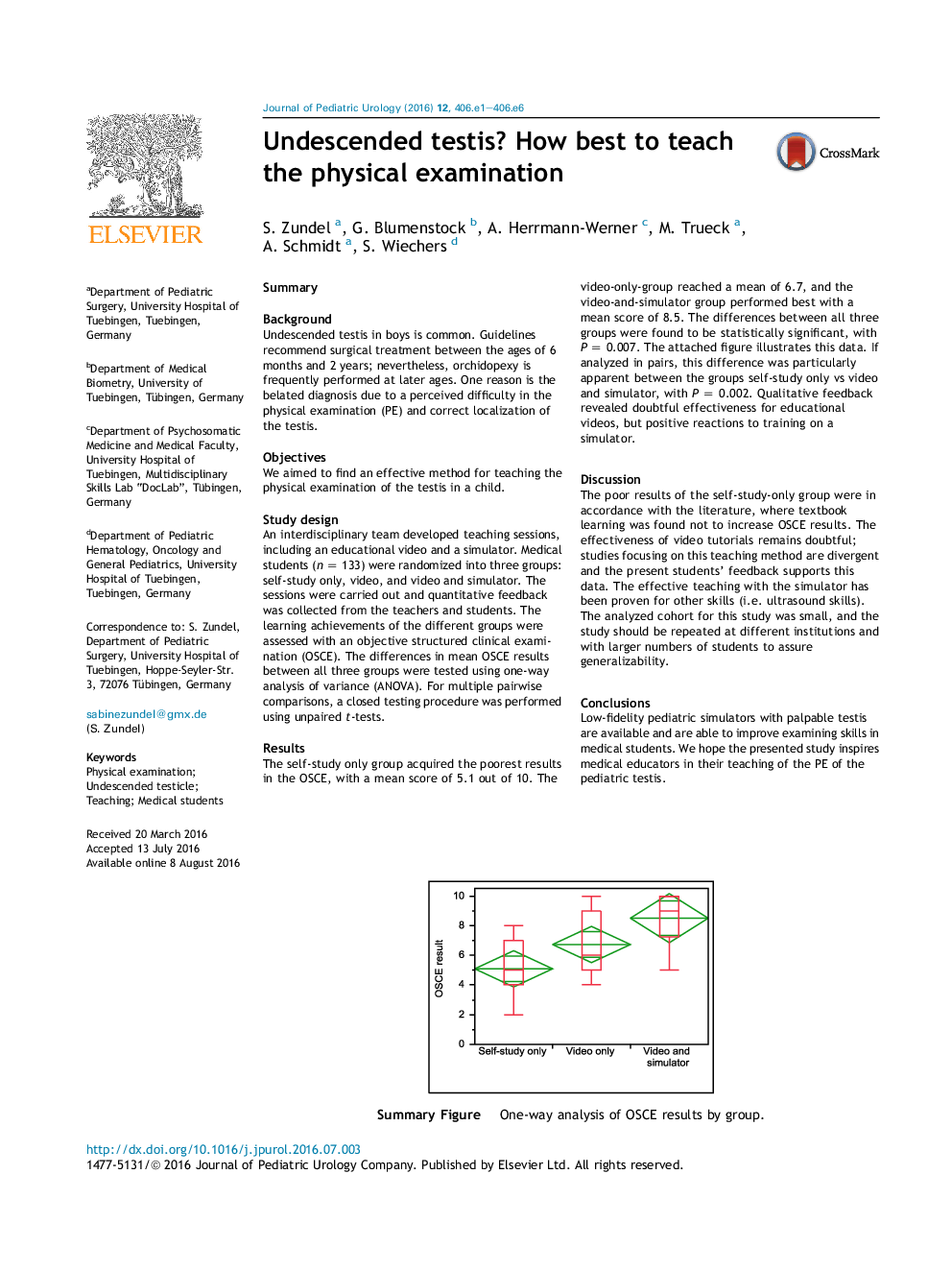
SummaryBackgroundUndescended testis in boys is common. Guidelines recommend surgical treatment between the ages of 6 months and 2 years; nevertheless, orchidopexy is frequently performed at later ages. One reason is the belated diagnosis due to a perceived difficulty in the physical examination (PE) and correct localization of the testis.ObjectivesWe aimed to find an effective method for teaching the physical examination of the testis in a child.Study designAn interdisciplinary team developed teaching sessions, including an educational video and a simulator. Medical students (n = 133) were randomized into three groups: self-study only, video, and video and simulator. The sessions were carried out and quantitative feedback was collected from the teachers and students. The learning achievements of the different groups were assessed with an objective structured clinical examination (OSCE). The differences in mean OSCE results between all three groups were tested using one-way analysis of variance (ANOVA). For multiple pairwise comparisons, a closed testing procedure was performed using unpaired t-tests.ResultsThe self-study only group acquired the poorest results in the OSCE, with a mean score of 5.1 out of 10. The video-only-group reached a mean of 6.7, and the video-and-simulator group performed best with a mean score of 8.5. The differences between all three groups were found to be statistically significant, with P = 0.007. The attached figure illustrates this data. If analyzed in pairs, this difference was particularly apparent between the groups self-study only vs video and simulator, with P = 0.002. Qualitative feedback revealed doubtful effectiveness for educational videos, but positive reactions to training on a simulator.DiscussionThe poor results of the self-study-only group were in accordance with the literature, where textbook learning was found not to increase OSCE results. The effectiveness of video tutorials remains doubtful; studies focusing on this teaching method are divergent and the present students' feedback supports this data. The effective teaching with the simulator has been proven for other skills (i.e. ultrasound skills). The analyzed cohort for this study was small, and the study should be repeated at different institutions and with larger numbers of students to assure generalizability.ConclusionsLow-fidelity pediatric simulators with palpable testis are available and are able to improve examining skills in medical students. We hope the presented study inspires medical educators in their teaching of the PE of the pediatric testis.Download high-res image (134KB)Download full-size imageSummary Figure. One-way analysis of OSCE results by group.