| Article ID | Journal | Published Year | Pages | File Type |
|---|---|---|---|---|
| 2955305 | Journal of the American College of Cardiology | 2007 | 8 Pages |
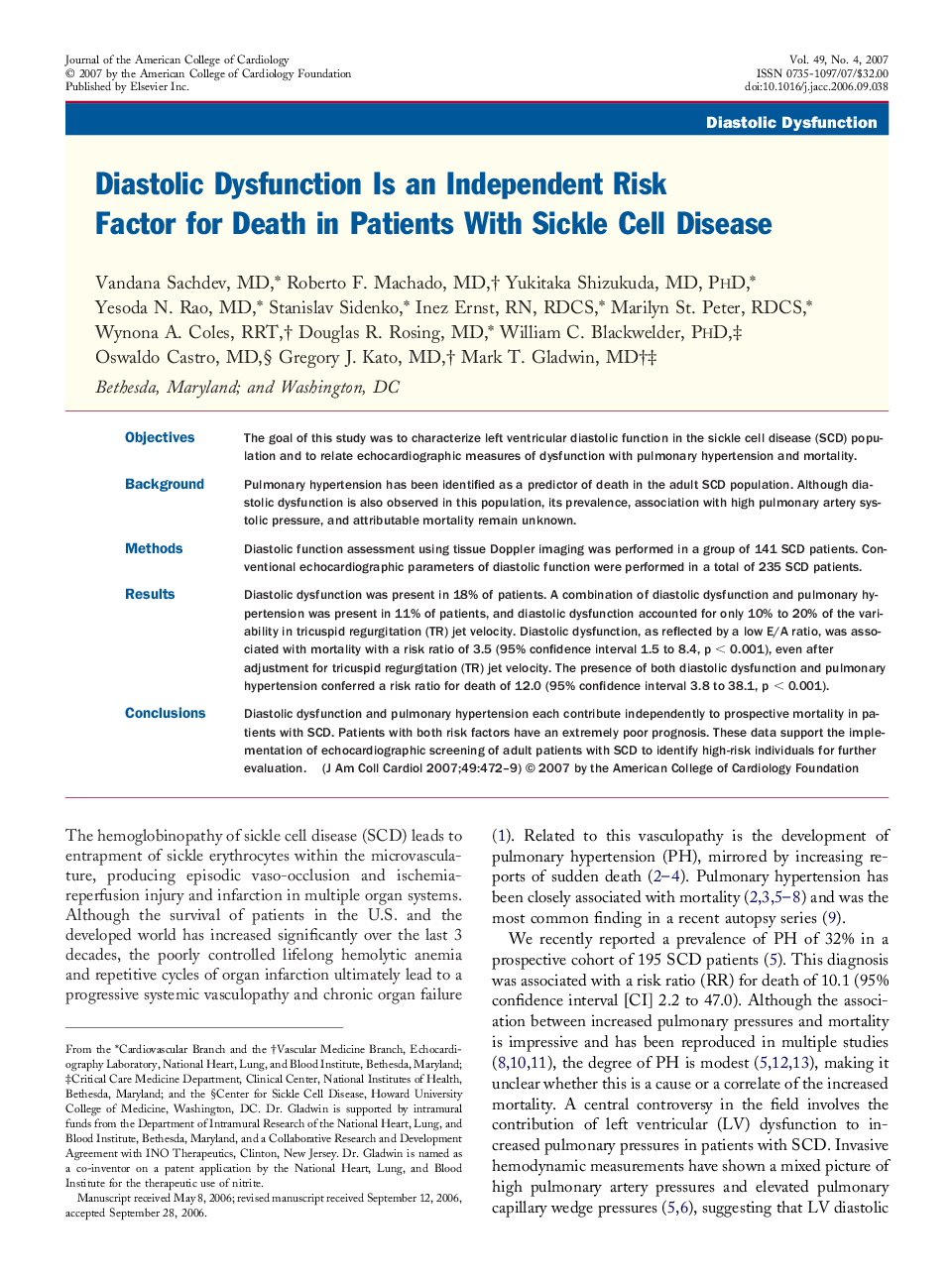
ObjectivesThe goal of this study was to characterize left ventricular diastolic function in the sickle cell disease (SCD) population and to relate echocardiographic measures of dysfunction with pulmonary hypertension and mortality.BackgroundPulmonary hypertension has been identified as a predictor of death in the adult SCD population. Although diastolic dysfunction is also observed in this population, its prevalence, association with high pulmonary artery systolic pressure, and attributable mortality remain unknown.MethodsDiastolic function assessment using tissue Doppler imaging was performed in a group of 141 SCD patients. Conventional echocardiographic parameters of diastolic function were performed in a total of 235 SCD patients.ResultsDiastolic dysfunction was present in 18% of patients. A combination of diastolic dysfunction and pulmonary hypertension was present in 11% of patients, and diastolic dysfunction accounted for only 10% to 20% of the variability in tricuspid regurgitation (TR) jet velocity. Diastolic dysfunction, as reflected by a low E/A ratio, was associated with mortality with a risk ratio of 3.5 (95% confidence interval 1.5 to 8.4, p < 0.001), even after adjustment for tricuspid regurgitation (TR) jet velocity. The presence of both diastolic dysfunction and pulmonary hypertension conferred a risk ratio for death of 12.0 (95% confidence interval 3.8 to 38.1, p < 0.001).ConclusionsDiastolic dysfunction and pulmonary hypertension each contribute independently to prospective mortality in patients with SCD. Patients with both risk factors have an extremely poor prognosis. These data support the implementation of echocardiographic screening of adult patients with SCD to identify high-risk individuals for further evaluation.