| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 2980147 | 1578601 | 2015 | 10 صفحه PDF | دانلود رایگان |
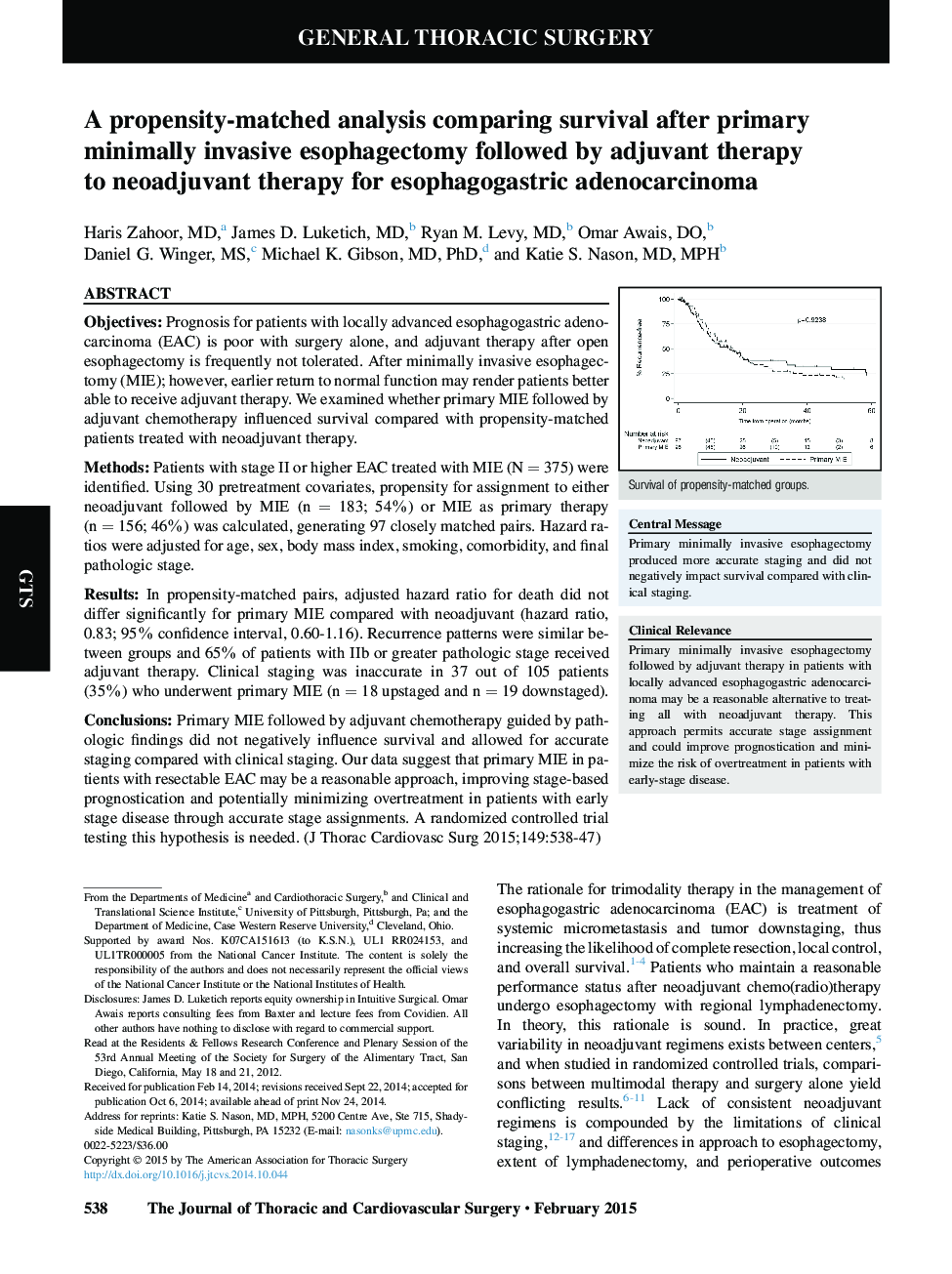
ObjectivesPrognosis for patients with locally advanced esophagogastric adenocarcinoma (EAC) is poor with surgery alone, and adjuvant therapy after open esophagectomy is frequently not tolerated. After minimally invasive esophagectomy (MIE); however, earlier return to normal function may render patients better able to receive adjuvant therapy. We examined whether primary MIE followed by adjuvant chemotherapy influenced survival compared with propensity-matched patients treated with neoadjuvant therapy.MethodsPatients with stage II or higher EAC treated with MIE (N = 375) were identified. Using 30 pretreatment covariates, propensity for assignment to either neoadjuvant followed by MIE (n = 183; 54%) or MIE as primary therapy (n = 156; 46%) was calculated, generating 97 closely matched pairs. Hazard ratios were adjusted for age, sex, body mass index, smoking, comorbidity, and final pathologic stage.ResultsIn propensity-matched pairs, adjusted hazard ratio for death did not differ significantly for primary MIE compared with neoadjuvant (hazard ratio, 0.83; 95% confidence interval, 0.60-1.16). Recurrence patterns were similar between groups and 65% of patients with IIb or greater pathologic stage received adjuvant therapy. Clinical staging was inaccurate in 37 out of 105 patients (35%) who underwent primary MIE (n = 18 upstaged and n = 19 downstaged).ConclusionsPrimary MIE followed by adjuvant chemotherapy guided by pathologic findings did not negatively influence survival and allowed for accurate staging compared with clinical staging. Our data suggest that primary MIE in patients with resectable EAC may be a reasonable approach, improving stage-based prognostication and potentially minimizing overtreatment in patients with early stage disease through accurate stage assignments. A randomized controlled trial testing this hypothesis is needed.
Journal: The Journal of Thoracic and Cardiovascular Surgery - Volume 149, Issue 2, February 2015, Pages 538–547