| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 2945686 | 1577160 | 2013 | 7 صفحه PDF | دانلود رایگان |
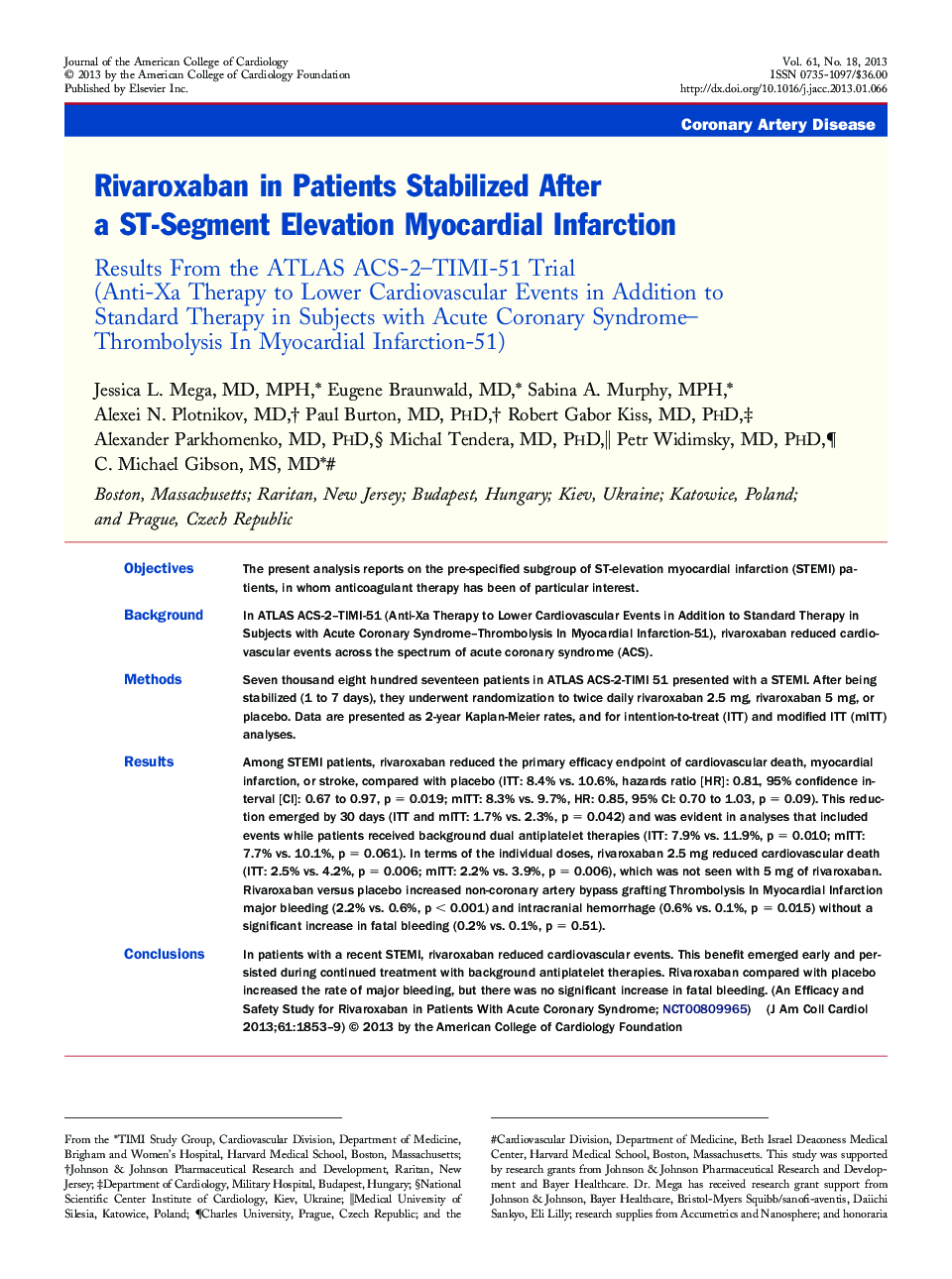
ObjectivesThe present analysis reports on the pre-specified subgroup of ST-elevation myocardial infarction (STEMI) patients, in whom anticoagulant therapy has been of particular interest.BackgroundIn ATLAS ACS-2–TIMI-51 (Anti-Xa Therapy to Lower Cardiovascular Events in Addition to Standard Therapy in Subjects with Acute Coronary Syndrome–Thrombolysis In Myocardial Infarction-51), rivaroxaban reduced cardiovascular events across the spectrum of acute coronary syndrome (ACS).MethodsSeven thousand eight hundred seventeen patients in ATLAS ACS-2-TIMI 51 presented with a STEMI. After being stabilized (1 to 7 days), they underwent randomization to twice daily rivaroxaban 2.5 mg, rivaroxaban 5 mg, or placebo. Data are presented as 2-year Kaplan-Meier rates, and for intention-to-treat (ITT) and modified ITT (mITT) analyses.ResultsAmong STEMI patients, rivaroxaban reduced the primary efficacy endpoint of cardiovascular death, myocardial infarction, or stroke, compared with placebo (ITT: 8.4% vs. 10.6%, hazards ratio [HR]: 0.81, 95% confidence interval [CI]: 0.67 to 0.97, p = 0.019; mITT: 8.3% vs. 9.7%, HR: 0.85, 95% CI: 0.70 to 1.03, p = 0.09). This reduction emerged by 30 days (ITT and mITT: 1.7% vs. 2.3%, p = 0.042) and was evident in analyses that included events while patients received background dual antiplatelet therapies (ITT: 7.9% vs. 11.9%, p = 0.010; mITT: 7.7% vs. 10.1%, p = 0.061). In terms of the individual doses, rivaroxaban 2.5 mg reduced cardiovascular death (ITT: 2.5% vs. 4.2%, p = 0.006; mITT: 2.2% vs. 3.9%, p = 0.006), which was not seen with 5 mg of rivaroxaban. Rivaroxaban versus placebo increased non-coronary artery bypass grafting Thrombolysis In Myocardial Infarction major bleeding (2.2% vs. 0.6%, p < 0.001) and intracranial hemorrhage (0.6% vs. 0.1%, p = 0.015) without a significant increase in fatal bleeding (0.2% vs. 0.1%, p = 0.51).ConclusionsIn patients with a recent STEMI, rivaroxaban reduced cardiovascular events. This benefit emerged early and persisted during continued treatment with background antiplatelet therapies. Rivaroxaban compared with placebo increased the rate of major bleeding, but there was no significant increase in fatal bleeding. (An Efficacy and Safety Study for Rivaroxaban in Patients With Acute Coronary Syndrome; NCT00809965)
Journal: Journal of the American College of Cardiology - Volume 61, Issue 18, 7 May 2013, Pages 1853–1859