| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 3851409 | 1598379 | 2006 | 9 صفحه PDF | دانلود رایگان |
عنوان انگلیسی مقاله ISI
Insulin Resistance, Inflammation, and Blood Pressure Determine Vascular Dysfunction in CKD
دانلود مقاله + سفارش ترجمه
دانلود مقاله ISI انگلیسی
رایگان برای ایرانیان
کلمات کلیدی
موضوعات مرتبط
علوم پزشکی و سلامت
پزشکی و دندانپزشکی
بیماریهای کلیوی
پیش نمایش صفحه اول مقاله
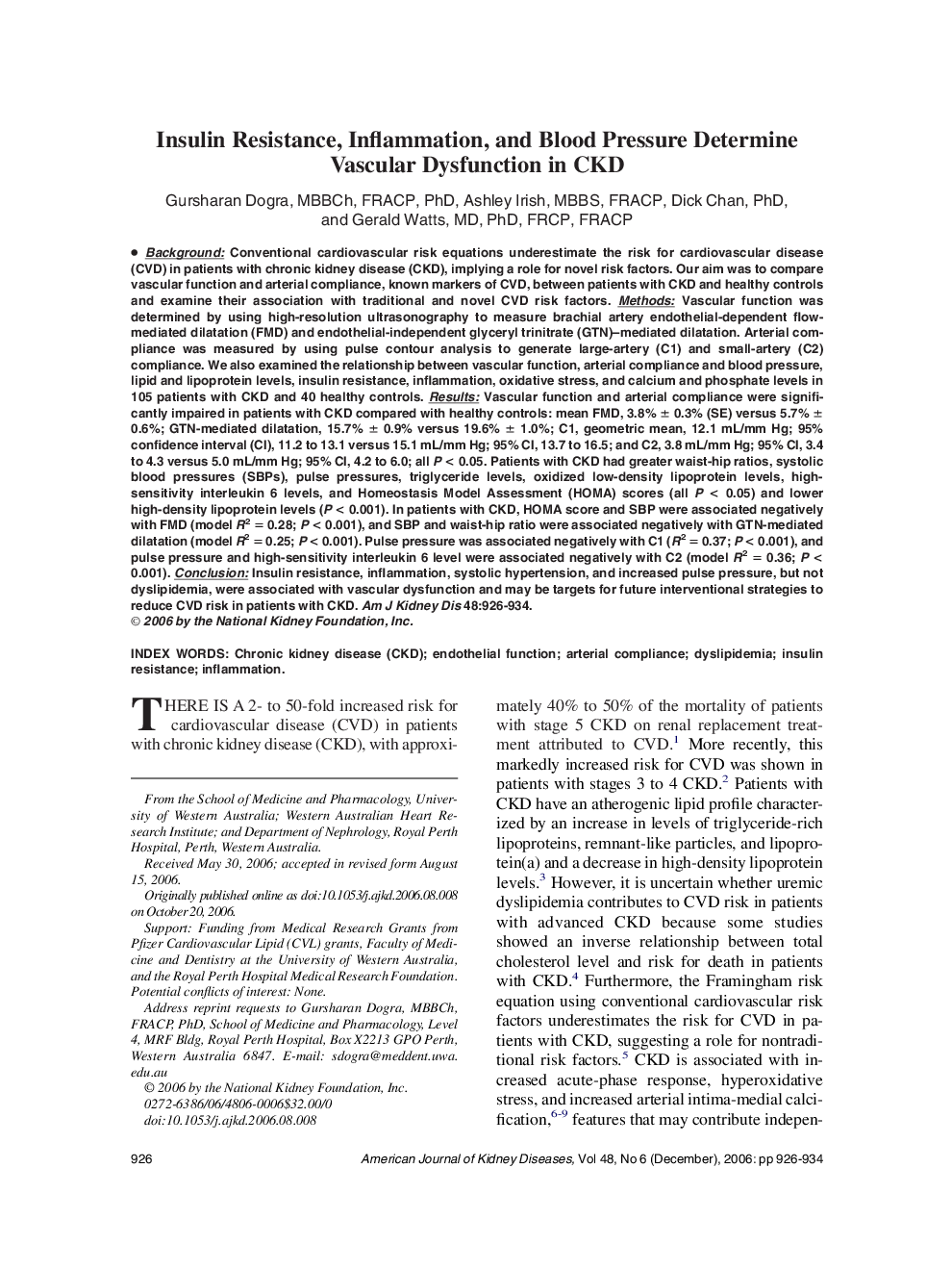
چکیده انگلیسی
Background: Conventional cardiovascular risk equations underestimate the risk for cardiovascular disease (CVD) in patients with chronic kidney disease (CKD), implying a role for novel risk factors. Our aim was to compare vascular function and arterial compliance, known markers of CVD, between patients with CKD and healthy controls and examine their association with traditional and novel CVD risk factors. Methods: Vascular function was determined by using high-resolution ultrasonography to measure brachial artery endothelial-dependent flow-mediated dilatation (FMD) and endothelial-independent glyceryl trinitrate (GTN)-mediated dilatation. Arterial compliance was measured by using pulse contour analysis to generate large-artery (C1) and small-artery (C2) compliance. We also examined the relationship between vascular function, arterial compliance and blood pressure, lipid and lipoprotein levels, insulin resistance, inflammation, oxidative stress, and calcium and phosphate levels in 105 patients with CKD and 40 healthy controls. Results: Vascular function and arterial compliance were significantly impaired in patients with CKD compared with healthy controls: mean FMD, 3.8% ± 0.3% (SE) versus 5.7% ± 0.6%; GTN-mediated dilatation, 15.7% ± 0.9% versus 19.6% ± 1.0%; C1, geometric mean, 12.1 mL/mm Hg; 95% confidence interval (CI), 11.2 to 13.1 versus 15.1 mL/mm Hg; 95% CI, 13.7 to 16.5; and C2, 3.8 mL/mm Hg; 95% CI, 3.4 to 4.3 versus 5.0 mL/mm Hg; 95% CI, 4.2 to 6.0; all P < 0.05. Patients with CKD had greater waist-hip ratios, systolic blood pressures (SBPs), pulse pressures, triglyceride levels, oxidized low-density lipoprotein levels, high-sensitivity interleukin 6 levels, and Homeostasis Model Assessment (HOMA) scores (all P < 0.05) and lower high-density lipoprotein levels (P < 0.001). In patients with CKD, HOMA score and SBP were associated negatively with FMD (model R2 = 0.28; P < 0.001), and SBP and waist-hip ratio were associated negatively with GTN-mediated dilatation (model R2 = 0.25; P < 0.001). Pulse pressure was associated negatively with C1 (R2 = 0.37; P < 0.001), and pulse pressure and high-sensitivity interleukin 6 level were associated negatively with C2 (model R2 = 0.36; P < 0.001). Conclusion: Insulin resistance, inflammation, systolic hypertension, and increased pulse pressure, but not dyslipidemia, were associated with vascular dysfunction and may be targets for future interventional strategies to reduce CVD risk in patients with CKD.
ناشر
Database: Elsevier - ScienceDirect (ساینس دایرکت)
Journal: American Journal of Kidney Diseases - Volume 48, Issue 6, December 2006, Pages 926-934
Journal: American Journal of Kidney Diseases - Volume 48, Issue 6, December 2006, Pages 926-934
نویسندگان
Gursharan MBBCh, FRACP, PhD, Ashley MBBS, FRACP, Dick PhD, Gerald MD, PhD, FRCP, FRACP,