| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 5718561 | 1607135 | 2017 | 6 صفحه PDF | دانلود رایگان |
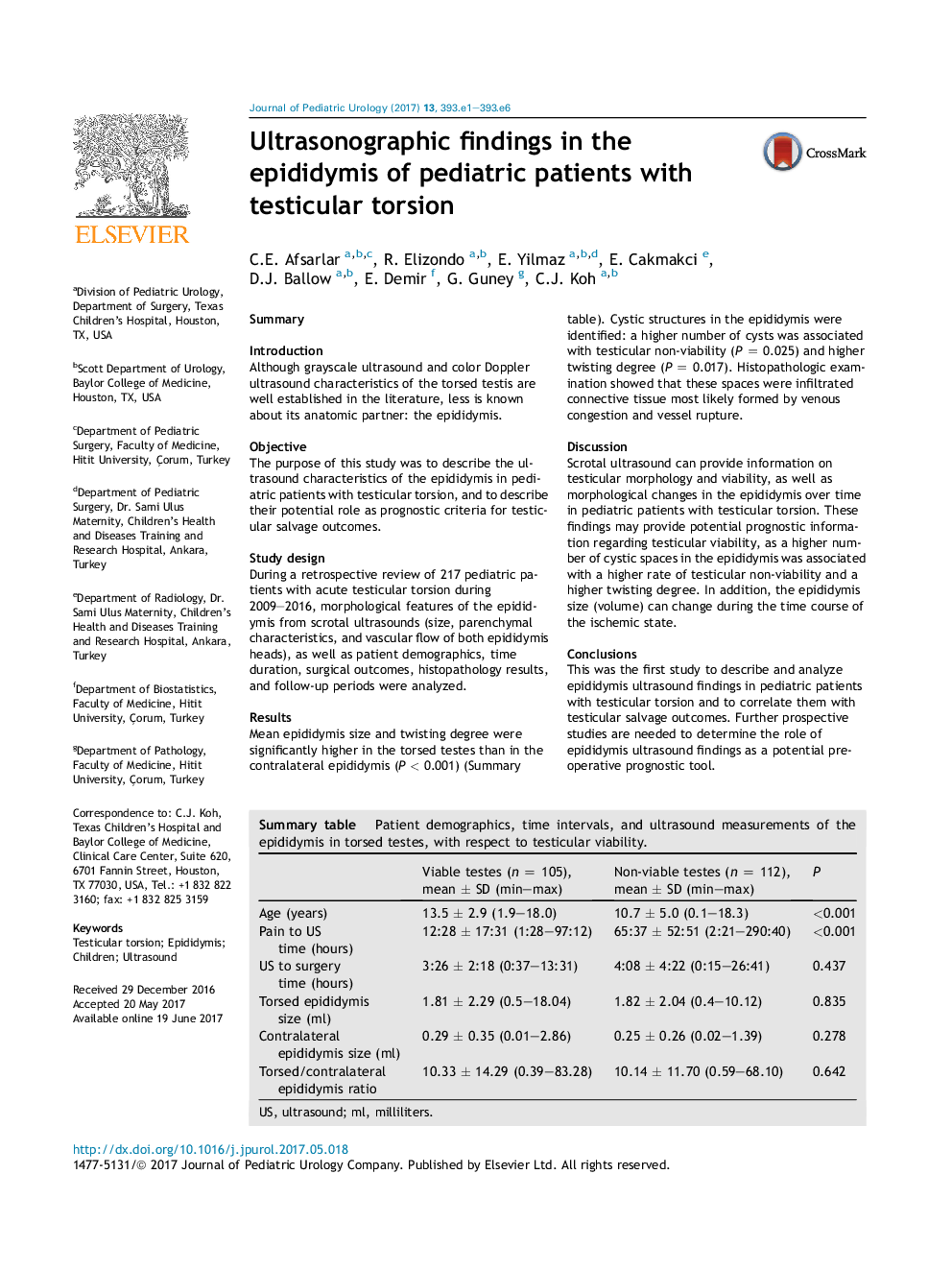
SummaryIntroductionAlthough grayscale ultrasound and color Doppler ultrasound characteristics of the torsed testis are well established in the literature, less is known about its anatomic partner: the epididymis.ObjectiveThe purpose of this study was to describe the ultrasound characteristics of the epididymis in pediatric patients with testicular torsion, and to describe their potential role as prognostic criteria for testicular salvage outcomes.Study designDuring a retrospective review of 217 pediatric patients with acute testicular torsion during 2009-2016, morphological features of the epididymis from scrotal ultrasounds (size, parenchymal characteristics, and vascular flow of both epididymis heads), as well as patient demographics, time duration, surgical outcomes, histopathology results, and follow-up periods were analyzed.ResultsMean epididymis size and twisting degree were significantly higher in the torsed testes than in the contralateral epididymis (P < 0.001) (Summary table). Cystic structures in the epididymis were identified: a higher number of cysts was associated with testicular non-viability (P = 0.025) and higher twisting degree (P = 0.017). Histopathologic examination showed that these spaces were infiltrated connective tissue most likely formed by venous congestion and vessel rupture.DiscussionScrotal ultrasound can provide information on testicular morphology and viability, as well as morphological changes in the epididymis over time in pediatric patients with testicular torsion. These findings may provide potential prognostic information regarding testicular viability, as a higher number of cystic spaces in the epididymis was associated with a higher rate of testicular non-viability and a higher twisting degree. In addition, the epididymis size (volume) can change during the time course of the ischemic state.ConclusionsThis was the first study to describe and analyze epididymis ultrasound findings in pediatric patients with testicular torsion and to correlate them with testicular salvage outcomes. Further prospective studies are needed to determine the role of epididymis ultrasound findings as a potential pre-operative prognostic tool.Summary table. Patient demographics, time intervals, and ultrasound measurements of the epididymis in torsed testes, with respect to testicular viability.Viable testes (n = 105), mean ± SD (min-max)Non-viable testes (n = 112), mean ± SD (min-max)PAge (years)13.5 ± 2.9 (1.9-18.0)10.7 ± 5.0 (0.1-18.3)<0.001Pain to US time (hours)12:28 ± 17:31 (1:28-97:12)65:37 ± 52:51 (2:21-290:40)<0.001US to surgery time (hours)3:26 ± 2:18 (0:37-13:31)4:08 ± 4:22 (0:15-26:41)0.437Torsed epididymis size (ml)1.81 ± 2.29 (0.5-18.04)1.82 ± 2.04 (0.4-10.12)0.835Contralateral epididymis size (ml)0.29 ± 0.35 (0.01-2.86)0.25 ± 0.26 (0.02-1.39)0.278Torsed/contralateral epididymis ratio10.33 ± 14.29 (0.39-83.28)10.14 ± 11.70 (0.59-68.10)0.642US, ultrasound; ml, milliliters.
Journal: Journal of Pediatric Urology - Volume 13, Issue 4, August 2017, Pages 393.e1-393.e6