| کد مقاله | کد نشریه | سال انتشار | مقاله انگلیسی | نسخه تمام متن |
|---|---|---|---|---|
| 2770661 | 1567807 | 2016 | 8 صفحه PDF | دانلود رایگان |
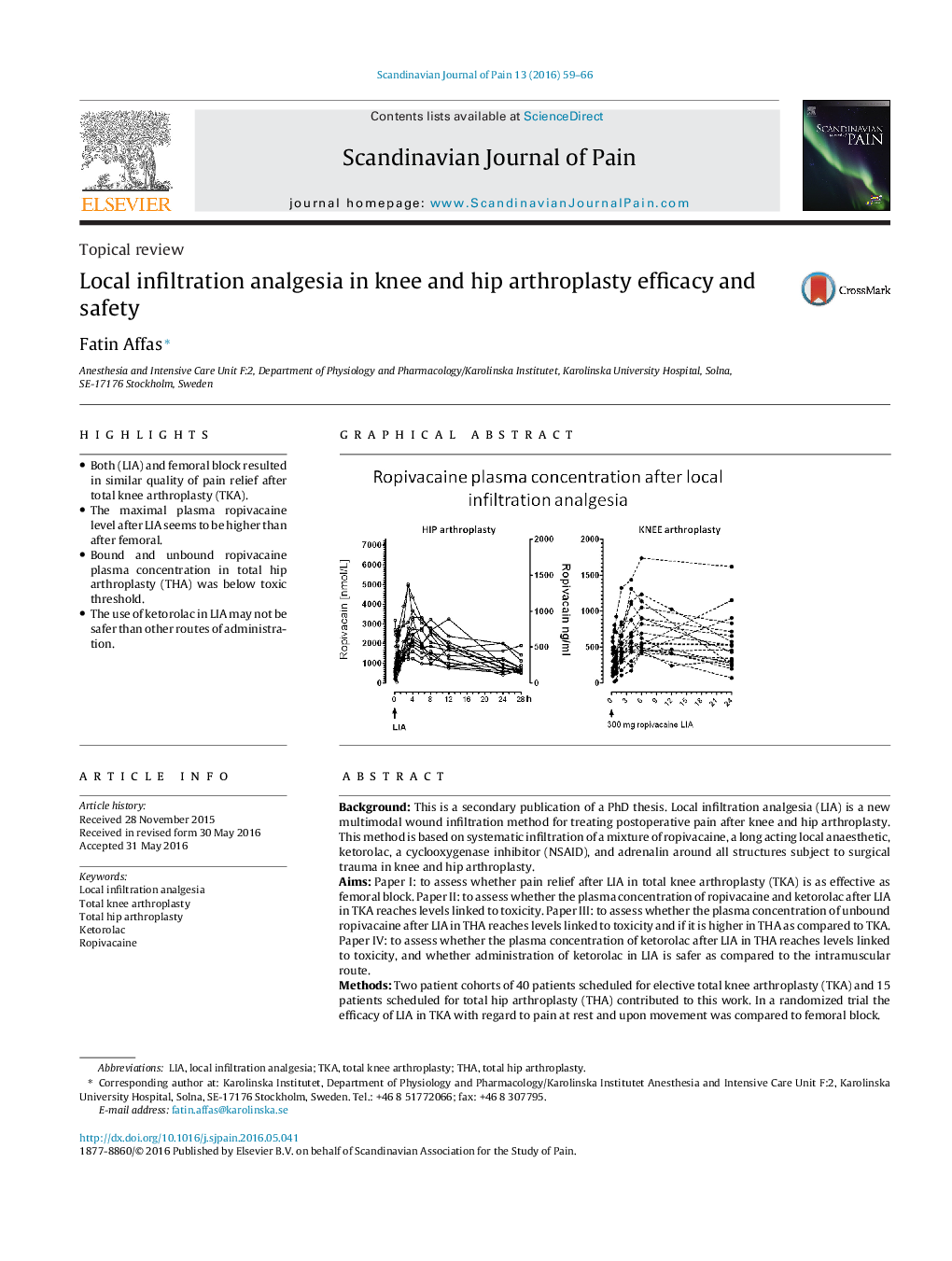
• Both (LIA) and femoral block resulted in similar quality of pain relief after total knee arthroplasty (TKA).
• The maximal plasma ropivacaine level after LIA seems to be higher than after femoral.
• Bound and unbound ropivacaine plasma concentration in total hip arthroplasty (THA) was below toxic threshold.
• The use of ketorolac in LIA may not be safer than other routes of administration.
BackgroundThis is a secondary publication of a PhD thesis. Local infiltration analgesia (LIA) is a new multimodal wound infiltration method for treating postoperative pain after knee and hip arthroplasty. This method is based on systematic infiltration of a mixture of ropivacaine, a long acting local anaesthetic, ketorolac, a cyclooxygenase inhibitor (NSAID), and adrenalin around all structures subject to surgical trauma in knee and hip arthroplasty.AimsPaper I: to assess whether pain relief after LIA in total knee arthroplasty (TKA) is as effective as femoral block. Paper II: to assess whether the plasma concentration of ropivacaine and ketorolac after LIA in TKA reaches levels linked to toxicity. Paper III: to assess whether the plasma concentration of unbound ropivacaine after LIA in THA reaches levels linked to toxicity and if it is higher in THA as compared to TKA. Paper IV: to assess whether the plasma concentration of ketorolac after LIA in THA reaches levels linked to toxicity, and whether administration of ketorolac in LIA is safer as compared to the intramuscular route.MethodsTwo patient cohorts of 40 patients scheduled for elective total knee arthroplasty (TKA) and 15 patients scheduled for total hip arthroplasty (THA) contributed to this work. In a randomized trial the efficacy of LIA in TKA with regard to pain at rest and upon movement was compared to femoral block.ResultsBoth methods result in a high quality pain relief and similar morphine consumption during the 24 h monitoring period. In the same patient cohort the maximal total plasma concentration of ropivacaine was below the established toxic threshold for most patients. All patients in the THA cohort were subjected to the routine LIA protocol. In these patients both the total and unbound plasma concentration of ropivacaine was determined. The concentration was below the established toxic threshold. As ropivacaine binds to α − 1 acid glycoprotein (AAG) we assessed the possibility that increased AAG may decrease the unbound concentration of ropivacaine. A 40% increase in AAG was detected during the first 24 h after surgery, however the fraction of unbound ropivacaine remained the same. There was a trend towards increased Cmax of ropivacaine with increasing age and decreasing creatinine clearance but the statistical power was too low to draw any conclusion. Administration of 30 mg ketorolac according to the LIA protocol both in TKA and THA resulted in a similar Cmax as previously reported after 10 mg intramuscular ketorolac. Neither age, nor body weight or BMI, nor creatinine clearance, correlates to maximal ketorolac plasma concentration or total exposure to ketorolac (AUC).ConclusionLIA provides good postoperative analgesia which is similar to femoral block after total knee arthroplasty. The plasma concentration of ropivacaine seems to be below toxic levels in most TKA patients. The unbound plasma concentration of ropivacaine in THA seems to be below the toxic level.ImplicationThe use of ketorolac in LIA may not be safer than other routes of administration, and similar restrictions should be applied in patients at risk of developing side effects.
Figure optionsDownload high-quality image (173 K)Download as PowerPoint slide
Journal: Scandinavian Journal of Pain - Volume 13, October 2016, Pages 59–66